Surviving Pandemics
The kidney community has often been noteworthy for its resilience and its ability to adapt in times of stress. This has never been more apparent than in its ability to respond during two different viral outbreaks over the last 75 years. At the time of the Hepatitis B virus outbreak in the 1960s, it threatened the very existence of UK kidney services. 60 years on, the COVID-19 pandemic threatened (and in some cases overwhelmed) health systems around the world.
Hepatitis B
There were outbreaks of blood-borne hepatitis in dialysis units from 1965 onwards, which had a devastating effect on the emerging programmes treating people with kidney failure.
The first was in Manchester in 1965, and this was followed by outbreaks in nine other units between 1966 and 1971. The most extensive was at Guy’s, the deadliest in Edinburgh.
It is not easy for us, sixty years on, to appreciate the severe challenge that hepatitis gave the kidney community.
- Patients and staff (including doctors, nurses and lab technicians) died, several nephrologists became severely ill. It took courage to come to work on the dialysis unit.
- The cause was at first unknown – the Australia antigen test was only just coming into clinical practice and hepatitis B had not yet been properly identified.
- Urgent measures were required, including segregation of infected patients, despite woefully inadequate facilities.
- The highest priority had to be given to transplanting all suitable infected patients or moving them to home HD (PD was not yet an established modality).
- Some dialysis units were closed temporarily, and in some cases, threatened with permanent closure. The development of long-term dialysis as a mainstream therapy came under existential threat.
It is easy in retrospect to see the risk that such epidemics might occur. Early dialysis units were severely overcrowded, machines and reusable dialysers were often shared between patients, blood transfusions were common.
The outbreaks were much more severe with higher mortality in some units; we can speculate now that this might be due to co-infection with hepatitis C (which had not yet been identified).
Confronted by the hepatitis crisis, an advisory committee chaired by Lord (Max) Rosenheim was established by the Department of Health, and the 1972 Rosenheim Report made recommendations which were universally implemented and remain the basis of the standard precautions mandated in kidney centres to this day.
COVID-19
In March 2020, the UK went into lockdown in response to an international health emergency. The COVID-19 virus, thought to have originated in China, was sweeping across the UK with real concerns that it would overwhelm health systems as it had done in other countries previously.
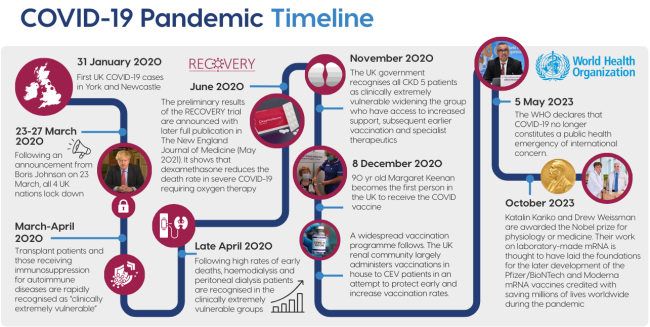
Over the next few weeks (March - April 2020), many late-stage kidney patients died, most kidney transplant programmes were paused, and kidney teams worked tirelessly. Patients with kidney transplants and those receiving strong immunosuppression for autoimmune diseases were rapidly recognised as being clinically extremely vulnerable to the effects of COVID-19. Approximately 25% of transplant patients who were infected died within 28 days of infection in the first wave. It soon became apparent that many more kidney patients were at risk.

Crowded haemodialysis units were badly affected. In the first and second waves of COVID, there was an estimated 25% unadjusted 28 day mortality rate for dialysis patients who contracted COVID, with those on dialysis for the longest and those not listed for transplantation being most vulnerable. In the first wave across all treatment modalities, those from more deprived areas and those with diabetes were more likely to be infected, and those over 80 were more likely to die. Infection control protocols were rapidly created to reduce the chances of spread. Outpatient appointments moved to a virtual provision.

Scientists strove to understand the virus, and a relaxation of research regulations, together with extraordinary dedication and effort from the entire medical and scientific community, led to the first glimmer of hope with the publication of the RECOVERY trial showing dexamethasone to reduce chances of death in severe cases. Acute kidney injury cases increased in the early days of the pandemic, possibly exacerbated by a need to “run dry” those whose lungs were overwhelmed by the virus. Concerns about overwhelming HD services led to acute PD enjoying a welcome renaissance.
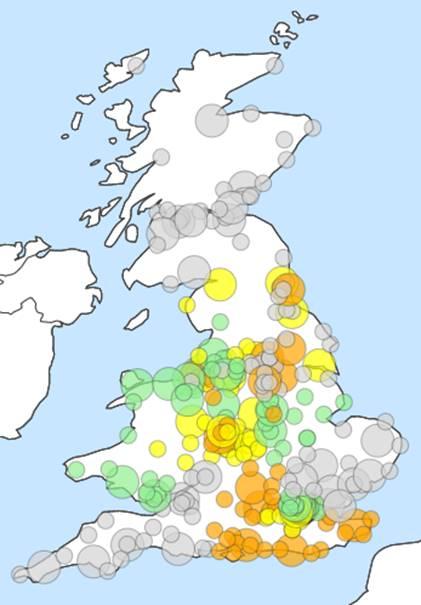
A breakthrough arrived in December 2020 when the first UK patient was vaccinated against COVID-19, and mass vaccination followed. Despite concerns about its rapid development and uncommon side effects such as coagulopathy and myocarditis, by August 2022, OpenSafely data suggested that 97% of its study population living with CKD stages 3-5 had received at least one vaccine, with delayed vaccine uptake in the young, minority ethnic groups and those living in deprivation. Data showing that those receiving immunosuppression for transplants or autoimmune disease made less good responses to the vaccine led to eligibility for extended vaccine regimes in these groups and early access to extended therapeutics if infected.
Over the next years, alpha, delta and omicron variants challenged our system whilst a plethora of complex anti-virals were developed, tested and used. The effects of illness and measures such as shielding leading to social isolation, as well as the huge backlog of routine NHS work that was delayed, left permanent scars on the community.
Staff were significantly affected. One study suggested that between the start of the pandemic and May 2021, 29% of kidney clinical staff were infected - with 36% of these experiencing symptoms of long COVID. Professionals lost loved ones and colleagues alike. The country applauded its key workers!

In the UK between the start of the pandemic and 5 May 2023, just under 227,000 people died, with COVID-19 listed as one of their causes of death - many more survived due to the hard work and courage of all those who contributed to their care in the pandemic.
The COVID inquiry continues to this day.
Yet for all its difficulties, the COVID pandemic precipitated extraordinary work. Never before had the scientific and medical community achieved so much progress against a disease in such a short time. Not only did the kidney community work tirelessly and with great courage, but it also pulled together bringing scientists, clinicians, patients and charities together with policy makers in unprecedented work. We hope that despite the sadness and the challenges, the kidney community will look back with pride.
