The Multi-Professional Team
This month we are reflecting on the contribution that multi-professional team members have made on the development of the kidney speciality, including dietitians, nurses, pharmacists, therapists, social workers and psychologists. Each of these professions has impacted on the care of people who live with kidney disease, by developing their own professional group and extending their professional role.
The Kidney Dietitian Specialist Group (KDSG), previously known as the Renal Nutrition Group (RNG) until November 2024 and earlier as the Renal Dialysis Group (RDG), holds the distinction of being the first specialist group of the British Dietetic Association (BDA). Formally established in 1970, the group initially concentrated on the medical and dietary management of people undergoing dialysis. Over time, its scope expanded to include renal transplantation and conservative management.

Some of the original RNG members. Left to Right: Betty Sloan Edinburgh RI, Marianne Vennegoor, St Thomas’s London, Alison Finch, F Prygrodzki, Nottingham General Hospital and Sue Bennett, Leicester General Infirmary
In 1997, the group was renamed the Renal Nutrition and in 2024, it became the Kidney Dietitian Specialist Group (KDSG) to align with the global move within nephrology to use kidney instead of renal. This rebranding also aimed to make the group's work and resources more relatable and understandable for patients and the wider public.
The KDSG has always championed an evidence-based approach to nutrition. Early influential publications, such as the European Dialysis and Transplant Association (EDTA) Proceedings (1968–1969) and Geoffrey Berlyne's edited volume, Nutrition in Renal Disease (1967), showcased the cutting-edge dietary practices of the time, particularly the Giordano-Giovanetti (GG) diet.
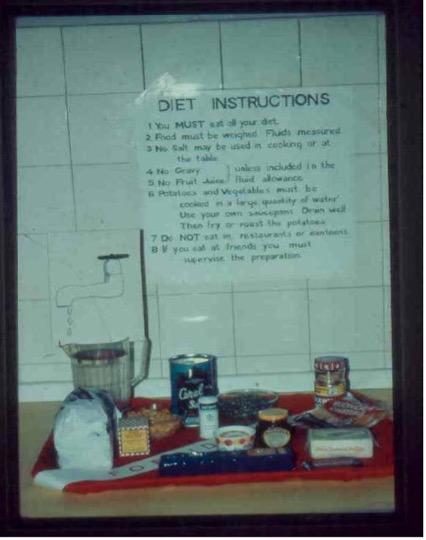
Poster from Middlesex hospital diet kitchen 1970s
Since then, the evolution of dietary advice for kidney care has been shaped by advancements in scientific research and clinical practice, for example the importance of improving nutritional intake before starting dialysis in the 1970s, which resulted in a gradual replacement of ultra-low-protein diets with maintenance diets providing 30–40g of protein per day. The 1980s and 1990s brought innovation in dietary guidance and resources. Key developments included the introduction of low-phosphate diets, the use of phosphate binders, and potassium exchange lists tailored to individual patient needs.

Dietitian (c. 1990) discussing low protein products with a patient
The KDSG has played a pivotal role in setting nutritional standards for kidney care with National Guidelines for Setting Standards of Dietetic Care for Adult Renal Patients, developed by the BDA-RNG and published in 1998, formalising these practices. By the early 1990s, the Renal Association and the Royal College of Physicians had highlighted the critical role of dietetic services, paving the way for workforce planning to address the growing needs of the chronic kidney disease (CKD) population.
In recent years, there has been a growing focus on kidney-friendly diets that emphasise plant-based nutrition. This shift reflects a broader understanding of the role of diet in promoting overall well-being, reducing complications, and potentially slowing the progression of kidney disease. Plant-based diets, which are naturally lower in phosphorus and protein while rich in fibre and antioxidants, offer significant benefits, including improved cardiovascular health and better metabolic control. Recent research has also highlighted the bioavailability of potassium in whole fruits and vegetables, which is often lower than in potassium additives, reducing concerns about excessive potassium intake from plant-based diets. Additionally, there is an increasing effort to reduce ultra-processed foods, which are often sources of hidden phosphate and potassium additives, further supporting improved kidney health.
Resources such as Kidney Care UK's Kidney Kitchen online recipe platform have been instrumental in providing patients with reliable and practical dietary options. Developed in collaboration with the KDSG, these recipes are carefully tested and approved to ensure they meet the specific needs of kidney patients. The KDSG continues to prioritise the development of resources that are inclusive and culturally appropriate, recognising the importance of addressing dietary practices across different cultural groups.
Renal dietitians are now able to train as supplementary prescribers, playing an increasingly vital role in patient care. This development offers significant benefits to both people living with CKD and the multidisciplinary team. For people with CKD, having renal dietitians who can prescribe, results in improved accessibility to medications and where diet and medication strategies align, more integrated care. In the multidisciplinary team, prescribing dietitians are demonstrating their confidence and competence to extend their roles, contributing to skill mix. Workforce planning should acknowledge this potential. To facilitate efficiency and increased autonomy, the BDA is currently working on a campaign to change legislation so that dietitians can prescribe independently. This will align dietitians with other non-medical prescribing professions. Support for this change will be sought from the kidney community.
Throughout its history, the KDSG has remained at the forefront of renal nutrition, continually adapting to advances in medical knowledge and the changing needs of patients. From the restrictive GG diet of the 1960s to the modern emphasis on plant-based nutrition and patient-centred care, improving both patient outcomes and quality of life.
Further information https://www.bda.uk.com/specialist-groups-and-branches/kidney-dietitian-specialist-group.html
Angeline Taylor, Team Lead Kidney Dietitian, Royal Devon University Healthcare NHS Foundation Trust, Exeter and Chair of the KDSG
Dr Barbara Engel, Post Registration Education Co-ordinator KDSG and Programme Director for Dietetics, University of Surrey
Nicki Ruddock, Advanced Clinical Specialist Dietitian, University Hospitals of Leicester NHS Trust
Marianne Vennegoor, Senior Renal Dietitian 1967-1999, formerly Guy’s and St Thomas’ NHS Foundation Trust
In the 1960s, renal units provided nurses with increased autonomy and responsibility, for example, cannulation of fistulae, roles which were not well-known in other specialities at the time. However, it was not until the early 1980s that registered nurses were offered specific training courses, such as the English National Board (ENB) 136, which lasted six months. Over the next twenty years, the profession of nursing developed hugely, with nurse prescribing in 2006, and all pre-registration nursing programmes becoming degree-level by 2009.
In 2025, the nursing team comprises a variety of nursing roles: consultant nurses, matrons, ward managers, specialist nurses (for example, advanced kidney care), and nursing associates (bridging the gap between health care assistants and registered nurses). Those working in non-registered nursing roles also make a huge contribution to the care team. Today, there are many exciting extended roles for kidney nurses, such as Advanced Clinical Practitioners (ACPs) who are educated to master’s degree level or equivalent, with the skills and knowledge to allow them to expand their scope of practice to better meet the needs of the people they care for.
Despite the huge development of the nursing profession over the past 75 years, professional support for nurses working in kidney care has been limited in recent years. The RCN Nephrology Nurses Forum was never influential and folded in the early 2000s, whilst the European Dialysis and Transplant Nurses Association/European Renal Care Association (EDTNA/ERCA) last held an annual UK meeting in 2018.
In 2018, the Association of Nephrology Nurses UK (ANN UK) was founded by three experienced renal nurses, Karen Jenkins, Helen Hurst and Paula Ormandy. ANN UK was developed under the umbrella of what was the British Renal Society (since merged with the Renal Association to form the UKKA), as they recognised a gap in professional support and a lack of a national voice for kidney care nurses. ANN UK is a non-profit membership organisation that aims to provide support for registered and non-registered nurses through education, mentorship, research, evidence-based practice, networking and collaboration with other renal and non-renal organisations.
Since 2018, ANN UK has had a number of key activities and successes:
- 2019 Executive Board formed. First SIGs: Research, Home Therapies
- 2020 Contributed to national guidance for providing haemodialysis in critical care, ensuring patient safety in haemodialysis units. Representation on national leadership groups, developed WhatsApp real-time support for lead nurses. Commenced Workforce planning update. AKI SIG formed
- 2021 Inaugural Virtual Conference. Commenced Mentorship programme. Regular column in Journal of Kidney Care. Judge for Renal Nurse of the Year award. Own website
- 2022 2nd Virtual Conference. HfRenDs Collaboration (Heart Failure, Diabetes Renal). ANN UK badged sessions at UKKW, EDTNA/ERCA affiliating with UKKA as a nursing group
- 2023 First in-person conference. Launch of ‘Enhancing Practice in Kidney Care’ e-learning modules. Joint working with PNNG, workforce planning. 2nd HfRenDs meeting. Move from SIGs to Communities of Practice (CoPs) to bring together ANN UK members with shared interests and expertise to collaborate, exchange knowledge, solve problems, and innovate in their field. Current CoPs include: Research, Home Therapies, Vascular Access, Advanced Kidney Care, Acute Kidney Injury, Anaemia, Haemodialysis, Transplant, Advanced Clinical Practitioners.
- 2024 2nd in-person annual conference. 3rd HfRenDs meeting. Expansion of CoPs & link with UKKA SIGs. KRUK research grants for nurses. Endorsement of education resources Collaboration with RCN
- 2025 3rd in-person Annual Conference. Workforce planning: Developing National competencies for registered nurses in Kidney Care. Education committee. Update of Enhancing Practice in Kidney Care’ e-learning modules. New CoPs: Transplant, Advanced Clinical Practice. KRUK Research grants round
Karen Jenkins, Consultant Nurse, Immediate Past President ANN UK
Prof. Nicola Thomas, Professor of Kidney Care, London South Bank University
The UK Renal Pharmacy Group (UK RPG) began in 1984 when 4 pharmacists met in Bristol. They invited a dozen companies who had a renal portfolio to support financially and continued to meet twice a year. In 1993, the first residential conference in Oxford was organised and this has become the heart of the RPG with a national conference each year.
In 1994, Ray Bunn from St Helier hospital, with support from the Committee, published the first renal drug handbook, and in 1998, Caroline Ashley and Aileen Dunleavy took over editing the handbook, which has become an internationally recognised guide to prescribing in patients with renal disease. In the early 2000s, the Introduction to Renal Therapeutics was written by UK RPG members and edited by Clare Morlidge and Caroline Ashley.
The UK RPG then went from strength to strength, with a restructure and integrated with the UKKA in 2021 and introduced a new logo to align with the UKKA. Members of the UK RPG have been involved with national programmes/projects and were part of each of the RSTP workstreams; provided advice for the Renal GIRFT report; input into relevant NICE guidance and have members of the NHSE renal CRG.
We have continued to grow our membership and have employed a specialist renal pharmacist to manage the renal drug database to ensure its succession, we support renal pharmacists nationally with monthly online Q&A meetings, Clare Morlidge became the first pharmacist UKKA president when she stepped down as chair of the UK RPG, and we present annually at the Clinical Pharmacy Congress.
We continue to progress renal pharmacy services and look forward to the next 40 years.
Further information https://www.ukkidney.org/rpg
Paul Clarke, Senior Specialist Renal Pharmacist, Oxford Kidney Unit
Clare Morlidge, Consultant Renal Pharmacist, East and North Hertfordshire NHS Trust, President UK Kidney Association.
Hayley Wells, Renal Pharmacist, Guys and St Thomas’s NHS Trust
The Association of Renal Technologists (ART) is the professional body representing all aspects of Renal Technology and supports all Renal Technologists who work either within the NHS or the private sector. The Association was formed in 1975, 27 years after the founding of the NHS. This was at the request of the Department of Health, following a couple of seminars that they had organised. The original intention was to promote and share experiences and ideas that were common to renal technicians who were working in dialysis and other aspects of renal medicine.
ART have never lost sight of the original ethos, that of being a conduit for the exchange of information and ideas, which are available to all. As with many other areas of medical devices technology, ART has seen huge leaps forward in all aspects of technology related to renal therapies and as such the renal technologist workforce has adapted and kept pace with continually developing and acquiring not only new technical knowledge and skills but also our knowledge of all aspects of renal therapies and services.
Further information https://www.renaltech.net/
Social workers have been a vital part of the multidisciplinary team in kidney care for decades, offering specialist psychosocial support to people living with kidney disease and their families. The National Renal Social Work Group was formally established in the mid-1990s, but our collective memory stretches back further - to the 1960s, when social workers sat on dialysis allocation panels, helping make difficult decisions about who could access life-saving treatment when NHS resources were scarce. Since those early days, the group has grown into a nationwide professional organisation that includes paediatric, young adult, and adult renal social workers, as well as social work associates, reflecting the need for lifelong support across the renal pathway. We are committed to supporting our members through education, training, peer support, and collaborative research, while also advocating nationally and regionally for the recognition of psychosocial needs in renal care. Our involvement in policy, service development, and patient-centred initiatives helps ensure that emotional, social, and practical needs are not overlooked. By bringing a social model of care into the medical setting, we strive to help people with kidney disease identify their strengths, navigate complex life challenges, and live as fully and independently as possible.
Further information https://ukrswg.co.uk/
Bethan Pettifer, Gweithiwr Cymdeithasol yr Uned Arennol, Liz Baker Unit, Morriston Hospital, Swansea
During the joint 2005 Renal Association/British Renal Society (BRS) Conference, a group of people with a keen interest in exercise-based rehab for people living with kidney disease approached the professional organisations to advocate for a dedicated and supported group to be established. This group would advocate for a growing number of health professionals working in both research and clinical practice-related activities in the field of renal exercise. In 2007, a BRS Renal Exercise Group was founded as a task and finish workstream. In 2010, we established the UKKRC Exercise and Lifestyle CSG with the first MPT lead of a CSG, and in 2014, the BRS Renal Rehab Network, with a seat on the BRS council, was developed. The great work of this network has continued into the new UKKA with the addition of a Living Well SIG to work with all members of the MPT to establish consensus on the recommendations for the RSTP and also to produce guidance and signposting to best practice. In 2024, the work of the UKKRC CSG and the BRS Rehab Network was combined to establish the Physical Activity and Wellbeing Rehabilitation Group (PAWR), the first joint working group to tackle both research and clinical implementation.
Further information https://www.kidneyresearchuk.org/research/research-networks/clinical-study-groups/physical-activity-rehabilitation-wellbeing-group/
Prof. Sharlene Greenwood, Professor of Exercise and Lifestyle Therapy and Consultant Physiotherapist, King’s Kidney Rehab Team, King's College Hospital, London

We may be tempted to think that attention to psychosocial issues in renal care, and the involvement of Psychologists in dialysis services, is a relatively recent development. However, the historical record tells a different story. As early as the 1960s, Clinical Psychologists were engaging with the emotional and psychological complexities of dialysis and transplantation. These early contributions suggest that the psychosocial dimensions of renal care were recognised from the outset, raising important questions about whether we have truly progressed or simply returned to what was already known.
Origins and Early Recognition (1960s to 1970s)
Renal Psychology emerged from the broader field of health psychology in response to growing awareness of the psychological toll of chronic kidney disease (CKD), dialysis, and transplantation. In the 1960s, Clinical Psychologists, Goodhue Livingston and Patricia Sand made some of the earliest contributions to the psychological understanding of dialysis by co-authoring seminal studies on patient selection and the emotional impact of treatment. Their work helped lay the foundation for integrating psychological assessment into renal care (Sand, Livingston, and Wright, 1966; Wright, Sand, and Livingston, 1966).
One of the first references to a Clinical Psychologist embedded in a renal team dates back to 1964, when a renal unit in Australia reported opening with a staff team that included a Psychiatrist, a Clinical Psychologist, and a Social Worker. In 1968, they published a paper in the British Medical Journal describing their work managing psychological issues in 47 patients with CKD and the challenges of screening 28 potential kidney donors (Cramond et al., 1968).
By the early 1970s, as dialysis became more widely available and life-sustaining for people with end-stage renal disease (ESRD), clinicians began to recognise the profound emotional and psychological challenges patients faced. These ranged from depression, anxiety, and cognitive difficulties to complex issues around adjustment, body image, and existential distress.
Expansion and Integration (1980s to 1990s)
During the 1980s and 1990s, renal units across the UK, the United States, and other high-income countries increasingly included Psychologists as part of the multidisciplinary team. Research during this period demonstrated that psychological distress was prevalent in this population and affected outcomes such as treatment adherence, transplant eligibility, and even survival. Clinical psychology began to be formally embedded in some renal services in the UK, although having a Psychologist in the service remained the exception rather than the rule.
The work of Clinical Psychologist Keith Nichols in Exeter during the 1980s was pioneering, and many of the challenges he described remain familiar today.
“Although the patients and partners were ‘surrounded’ by caring staff, in many subtle ways they were quite alone with their distress. They were cared for physically, but there was little effective psychological care” (Nichols and Springford, 1984).
“It was obvious that this lack of psychological care was not something that a lone, part-time Clinical Psychologist could do much about… Further, what we were noticing was not mental health issues needing treatment, but more emotional disarray provoked by poor information exchange and lack of emotional care” (Nichols, 2005).

Keith developed ways of working that set the model for Renal Psychology as a specialism. His approach to psychological care included regular monitoring of psychological state and routines to check and amplify the information held by patients, helping to maintain realistic expectations. This was combined with emotional care as needed, and referral for therapy to a Clinical Psychologist where appropriate. The Psychologist was seen as trainer, supervisor, and available therapist within the model (Nichols, 1993).
Consolidation and Growth (2000 to 2025)
Between 2000 and 2025, Renal Psychology underwent consolidation, expansion, and increasing recognition within multidisciplinary renal services. Early in this period, Psychologists often worked in relative isolation, with limited national guidance and wide variation in service provision across the UK and internationally. However, growing awareness of the psychological impact of kidney disease, particularly the demands of dialysis, transplant, and end-of-life care, led to a gradual increase in dedicated Psychology posts (including Clinical, Counselling and Health Psychologists) within renal teams. Psychologists in nephrology departments began to focus on staff consultation, and training in addition to assessment and therapeutic interventions.
In the UK, the need for psychological support in renal services has been highlighted in national policy and research documents, including the UK Renal Psychosocial Workforce Mapping Exercise (2018), Caring for People with Kidney Disease: Psychosocial Health, A Manifesto for Action (2022), and Addressing the Mental Health Challenges of Life with Kidney Disease (2023). Nevertheless, provision has remained uneven, with ongoing advocacy for equitable access to psychological care across renal units. Psychologists have played key roles in shaping service design, leading quality improvement projects, and influencing national strategy on kidney care.
The British Psychological Society (BPS) Renal Network was established around 2003 to provide a dedicated forum for Psychologists working in renal settings across the UK. This network facilitates peer support, professional development, and the exchange of research and Clinical innovations. It has been instrumental in raising the profile of Renal Psychology within the broader psychology community and in influencing national policy and commissioning strategies. The network offers members opportunities to contribute to training, guidelines, and service improvement initiatives tailored to the psychological needs of renal patients.
Today’s Renal Psychology
In 2025, Renal Psychology is no longer seen as an optional extra. It is recognised as a core component of high-quality kidney care. Nevertheless, challenges remain in achieving consistent staffing levels, equitable access, and broader recognition of the complexity of psychological work in this setting. Increasingly, Renal Psychologists contribute to leadership, research, service development, and training, with a growing presence at national forums and in policy discussions shaping the future of kidney care.

Renal psychology remains a specialist and deeply relational field, grounded in witnessing distress, fostering resilience, and holding space for the full human experience of chronic illness. However, the number of psychologists working in this area in the UK remains relatively small. At the national Renal Psychology study day in January 2025, around 30 psychologists attended, and there are currently approximately 40 posts across adult and paediatric renal psychology services nationwide.
Though small in number, Renal Psychologists make an essential contribution to kidney care, and the value of their work is increasingly recognised as services strive to meet the complex needs of patients and families.
Dr Emma Coyne, Consultant Clinical Psychologist
